The modern healthcare landscape is always evolving – especially when it comes to sterile processing. Here are five trends that are reshaping the sterile processing landscape in the years ahead.
Of all the wings, specializations, and departments in any given hospital across the world, the sterile processing department (SPD) or central sterile supply department (CSSD) might just be the one that connects them all.
Because nearly every medical instrument from every department must pass through SPD/CSSD at some point in its life, it is even more necessary for this department to be performing at the absolute highest level possible. If anything goes wrong at the sterilization stage, that problem will only domino into a full collapse later on in the instrument’s journey.
Yet, things – as they tend to do – have been changing. Technology is advancing, more research has exposed flaws and advantages in current sterile processing techniques, and even the way hospitals are funded and run is constantly undergoing development. Not to mention, the pandemonium of the Covid-19 pandemic is hardly out of the rear-view mirror’s gaze. So, the pressure for SPDs to commit to consistency, organization, and standardization amid each new change is on.
Everyone knows that you can’t stay at the top of your game if you don’t know the score. So, here are five trends in sterile processing that every clinician should be aware of:
Trend #1: Prioritizing high-level disinfection
Arguably the biggest topic of conversation in instrument/equipment processing right now is high-level disinfection (HLD). According to Steris Healthcare, HLD is “the complete elimination of all microorganisms in or on an instrument, except for small numbers of bacterial spores. The FDA further defines a high-level disinfectant as a sterilant used for a shorter contact time to achieve a 6-log1 kill of an appropriate Mycobacterium species.”
The concepts of quality and assurance must be applied to all the processes of disinfection and sterilization.
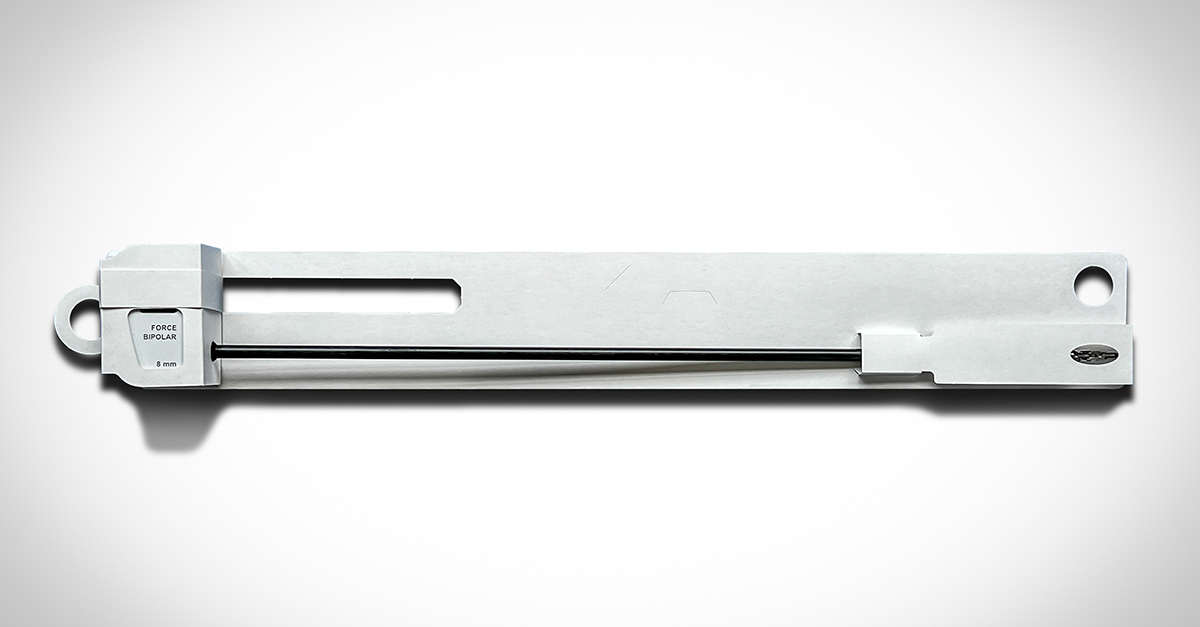
Guy Phipps, RN, BSN, MBA, CNML, Director of Perioperative Services, Cath Lab, GI & ASC Administrator and cofounder of SterileBits, says to achieve this, the industry needs consistency in how instruments are delivered to the operative field. One of the best ways to do this, he argues, is to use an instrument protector card, which has more structure than other kinds of instrument protectors on the market.
“Everything that we can do to ensure consistent high-level instrument delivery will lead to a higher standard of patient care and, from a clinician’s point of view, organization,” said Phipps.
Trend #2: More tactful use of and care for robotics

One of the most recent advancements in sterile processing and healthcare as a whole has been the development of robotic surgical instruments. The implementation of robotic surgical instruments has been one of the most rapidly accepted (and the most rapidly evolving) advancements that the healthcare industry has ever seen. After all, the first robot ever used for surgery, a PUMA 200 that was used for needle placement in a CT-guided brain biopsy, occurred less than 40 years ago (Jay Shah, BS, Arpita Vyas, MD, and Dinesh Vyas, MD, MBBS, MS, FICS, FACS). In 2024, the use of robotics is common practice. Still, the way that robotics are used is changing every day.
“When robotics entered the scene 20 years ago, the industry tried to do everything with a robot before we narrowed it down to what actually provides a better outcome for patients. That allowed it to become the consistent tool it is today,” said Phipps. “The next step is to make sure we are sterilizing and caring for robotic instruments in an equally consistent manner. Public demand wants the latest and best for patients and we need to be able to deliver care in that way. Making sure we have consistency in the equipment that’s coming out of SPD is a high, high focus. Standardizing the use of instrument protector cards is a great way to do that.”
Trend #3: Centralized sterile processing
In recent years, it has become more and more popular for hospitals and hospital networks to not actually sterilize equipment within the walls of the hospital. Rather, many institutions, especially in the Midwest and the East Coast of the United States, are moving towards centralized sterile processing. In this model, a regional processing unit is an entirely separate building to which everything is sent.
“What this helps do is create consistency,” said Phipps. “Because, traditionally, if each hospital has its own SPD, that leads to a greater diversity of sterilization techniques and practices. If all sterilization happens out of the same place, it creates consistency, which minimizes problems and points of confusion that can arise without that level of organization.”
Trend #4: World-wide push for sustainable practices in hospitals
Sustainability is a major source of conversation in many hospitals today. Take it from The Joint Commission, the nation’s oldest and largest standards-setting and accrediting body in health care, who launched a Sustainable Healthcare Certification (SHC) program effective January 1, 2024.
Waste is hardly avoidable, especially where sterilization is concerned. However, there are plenty of ways to significantly reduce the amount of waste that the healthcare industry generates.
One such approach is to make sure that everything that can possibly be recycled, is. That’s why instrument protector cards by SterileBits are 100% recyclable.
Another way to implement sustainable practices in hospitals is to protect what you have so that you don’t need more of it. By using an instrument protector card, for example, not only is the surface area of surgical instruments more exposed to sterilant than with a rubber tip or other kind of instrument protector, it also protects the instrument from damage. This means that an instrument can be of use for its entire useful life without being replaced by another. The more we use what we have, the less waste we generate in the long run.
Read more about instrument protection and sustainability in sterile processing here.
Trend #5: New (and improved) instrument protection
Several years back, SterileBits conducted a study with the V.P. of The Musculoskeletal Infection Society, Dr. Antonia Chen, and chemist Noreen Hickok, Ph.D. The doctors designed the protocol and conducted the study at the Rothman Orthopedic Institute. The study compared the sterility of orthopedic drill bits in their reprocessed consigned trays to prepackaged sterile drill bits. In each of four separate test events, 25% of the drill bits pulled from consigned trays had living fungus and bacteria on them.
That can only mean one thing — what we’re doing now is just not good enough.
So, what do we do instead?
Phipps offers that the solution to this problem can be found in using instrument protector cards instead of rubber tip protectors or peel pouches alone. While rubber tips obscure parts of equipment from sterilization, instrument protector cards by SterileBits maximize the amount of space that is in contact with sterilant.
Additionally, instrument protector cards by SterileBits add extra rigidity to the pack and place a barrier between an instrument’s delicate edges and the pack. This means the instruments are safeguarded against damage and breach of the sterile barrier. So, when it gets in the hands of a clinician, that clinician can be as certain as humanly possible that the instrument is sterile and ready for use.
SterileBits: A New Future for Sterile Processing
To read stories similar to this one, visit the SterileBits blog.
To learn more or find a distributor near you, visit www.sterilebits.com.

