To be at their best, SPDs and ORs must communicate. Sterile Technician Elias Cantu takes us through what happens when the departments don’t talk and how he promotes collaboration through what he calls “intangibles”.
Houston, Texas – In surgery, every minute matters.
Every moment a patient is under anesthesia and open on a table – even for a minimally invasive surgery (MIS) – is a vulnerable one. Many studies, including Cheng H, et. al.’s study, Prolonged operative duration is associated with complications: a systematic review and meta-analysis., published in the Journal of Surgical Research on April 24, 2018, confirm that prolonged operative duration is, indeed, associated with an increased risk of complications.
Because of this, reducing surgical duration is one of the primary initiatives pursued by surgical teams and researchers.
Who among any surgical team hasn’t been asked the question: How can we be more efficient?
Well, one path toward efficiency begins long before the team is assembled, and the operating room (OR) is prepared. Depending on the hospital, it might even begin off-site.
You’ve probably guessed we’re referring to the work of the sterile processing department (SPD).
“They call us the heartbeat of the hospital for a reason,” said Elias Cantu, sterile processing technician at Texas Children’s Hospital in Houston. “Without us, nothing would run. I take a lot of pride in knowing that what I do is important.”
Cantu isn’t only a sterile processing technician. He’s also an on-site specialist. In this role, Cantu acts as a liaison between the operating room and the sterile processing department at Texas Orthopedic.
This position has given Cantu an experience that very few actually have; he’s a first-hand witness to the full journey of a surgical instrument from sterilization to use. Though sterile technicians and surgical teams hold the very same instruments in their hands each day, it’s usually rare that they ever meet in person, let alone see each other work.
Naturally, this creates a barrier between the departments. That’s exactly the gap Cantu strives to bridge.
“I act as the liaison between SPD and the OR,” said Cantu. “It’s so illuminating seeing both sides of the process. My work ensures things run much more smoothly. I’m also fortunate enough to get to take what I learned working with the OR team and carry that over to the SPD at Texas Children’s. I really believe that knowing what’s going on in the OR leads to me doing a better job as a technician.”
It’s not hard to understand how context such as this is key for building mutual understanding, but it does even more than that. This deep understanding of what’s happening in SPD and in the OR can lead to important structural and operational changes.
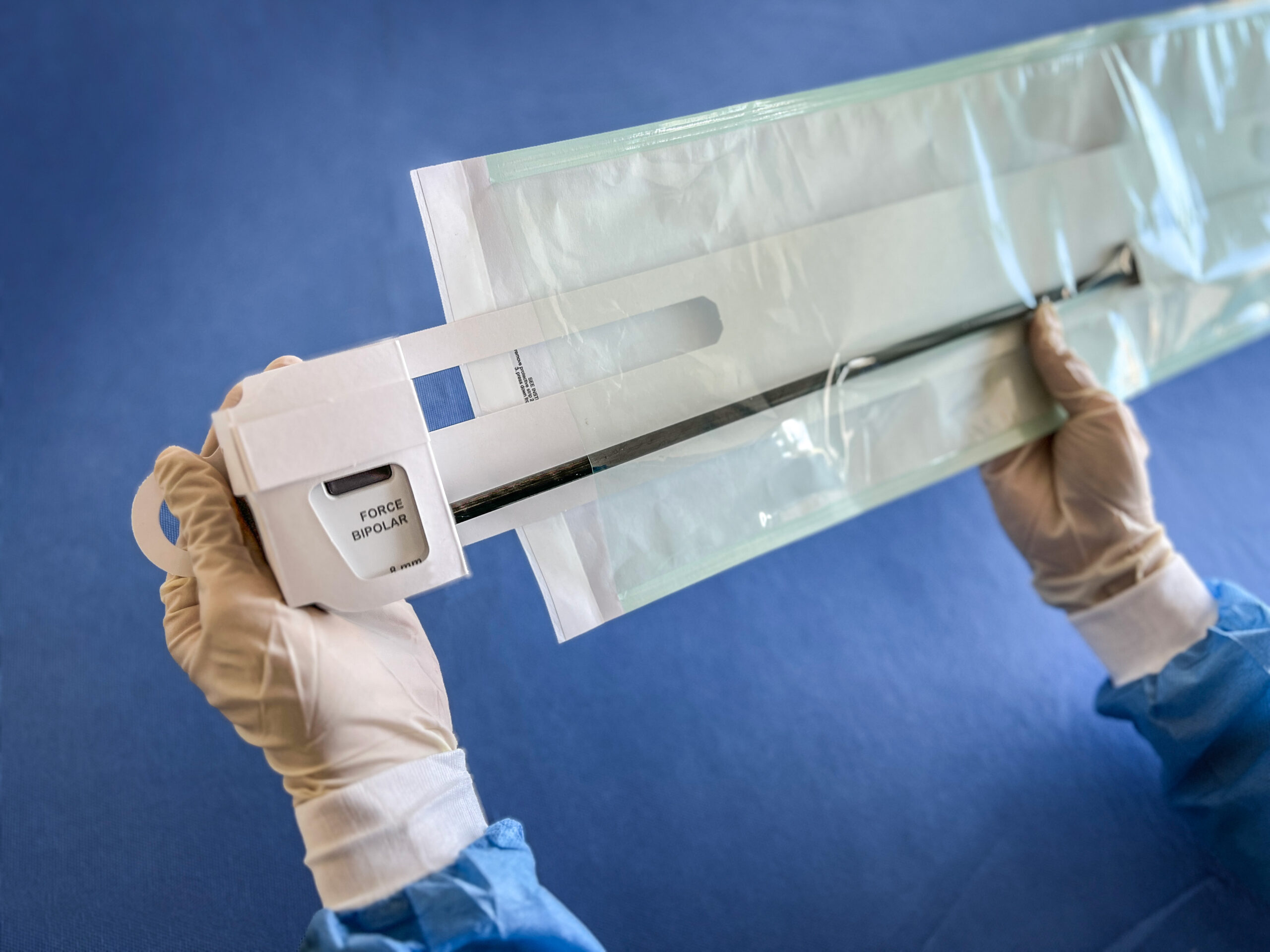
Take, for example, packaging for sterile instruments. Though there’s a standard process for both sides of the equation – sterilize, place an instrument in the pouch, and send it off to be used in the OR, where OR staff open the pack and place it within the sterile field – there’s also a lot that happens in between. Tumbling and tossing of instruments is only natural when transporting materials in a high-intensity environment.
Without the proper protection, that tossing and turning can lead to real problems for the OR staff. In fact, these problems have become so pervasive that AAMI updated its guidelines for transporting sterile devices in 2025.
“I’ve seen with my own eyes how important it is to ensure the integrity of peel packs,” said Cantu. “Depending on the hospital I’m working in, sometimes the OR receives peel packs where the instrument itself tore its pouch because it was loose inside. When that happens, the OR staff have to completely de-gown and start their sterilization process over. Meanwhile, we have to go find a new instrument.”
“Not only is it a pain, but it really prolongs how long the patient is under anesthesia, and the goal is to get them up as soon as possible,” continued Cantu.
The good news is: there’s a solution.
“Recent advancements in antiseptic presentation, such as using an instrument protector card to hold a sterile instrument in place, have really helped,” said Cantu. “We use the SterileBits instrument protector cards at Texas Children’s. Before using those, we had to re-pack instruments often. We experimented with a lot of tip protectors, but the SterileBits solution is the best.”
“For one, it’s very easy to use. Secondly, it makes life so much easier for the OR staff,” said Cantu. “Those are the kind of things you notice – and the problems you can solve – when you see things from both the OR and SPD perspective.”
The Importance of Intangibles: Cantu’s “Why”
Operational fixes such as this are key to both patient safety and hospital efficiency. That being said, Cantu argues there’s also a lot of value in what he calls “intangibles”.
“Intangibles are things that you can’t really see, but at the end of the day, you feel when they’re done,” said Cantu. “It might not go on my productivity sheet, but things like answering phone calls, giving advice and guidance to newer technicians, and helping out your team by having a good attitude go such a long way. At the end of the day, I want to go home knowing I did right by my title and my team.”
For Cantu, this drive comes from a deep understanding of the consequences of his work.
“People want to help. That’s what we’re in healthcare for, and that’s why someone joins sterile processing. The patient deserves your best every single day,” said Cantu. “I can honestly say every time I come into any department, I want to give my best foot forward because that’s what I would want if I were on the table.”
SterileBits: Give Your Best
To read more stories similar to this one, visit the blog on www.SterileBits.com and follow SterileBits on LinkedIn.