
Miscommunication and human error just might be two of the most frustrating challenges that a sterile processing educator can try to solve. Well, unless you’re Anna Castillo-Gutierrez, Sterile Processing Educator at Texas Children’s Hospital. Here’s how she does it.
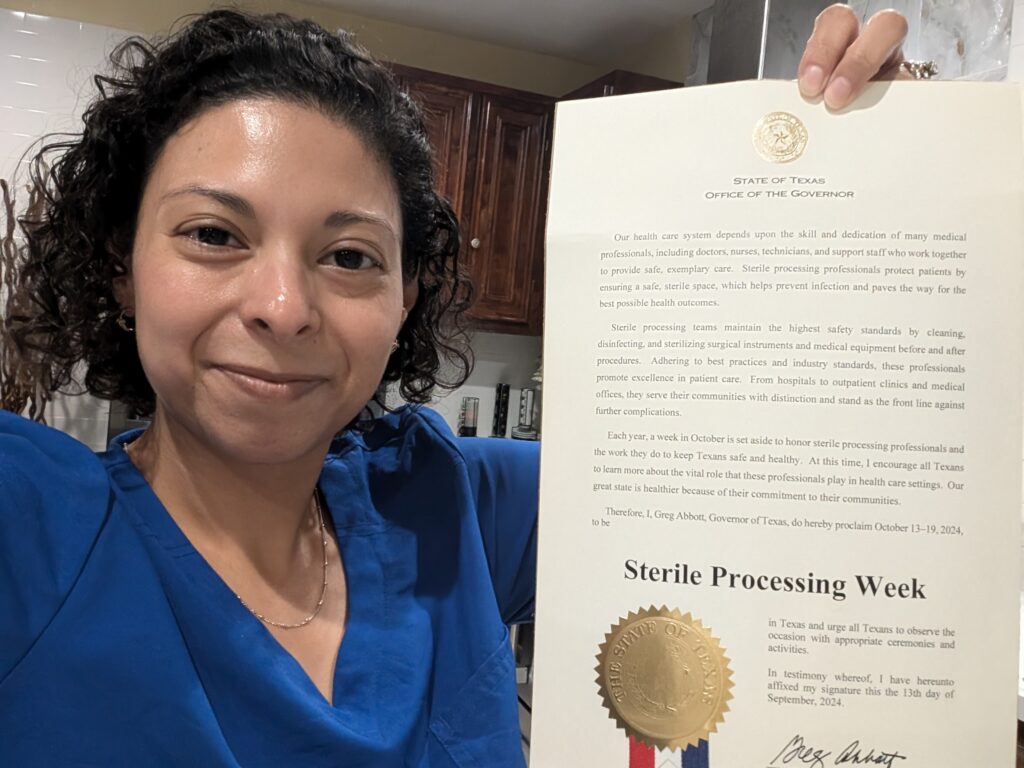
Houston, Texas – To know where you’re going, you have to look back at where you came from. That’s why when Anna Castillo-Gutierrez, CRCST, CSPDT, CHL CIS, CFER, Sterile Processing Educator at Texas Children’s Hospital, envisions the future of sterile processing, she considers how it began.
Before the Industrial Revolution, the siloing of healthcare jobs such as nursing and sterile processing was much less common than it is today. Nurses, for example, were previously responsible for surgery, the patient, and reprocessing instruments – duties that are now three separate positions. “They handled absolutely everything,” said Castillo-Gutierrez.
Then, in congruence with the rise of the assembly line, generalized healthcare positions became even more specialized. “We started to see this trend of sub-nursing units, where nurses would either be an operating room (OR) nurse or a circulating nurse, etc.,” said Castillo-Gutierrez. “The sterile processing department (SPD) has followed a similar pattern. Nowadays, SPD technicians, managers, instrument specialists, coordinators, and educators all have different roles.”
“Ultimately, this trend towards specialization helps grow the department and ensure things are done the way they should be,” said Castillo-Gutierrez. “But it does create its own set of problems.”
 Problem number one: effective collaboration. Specialization, while critical for the ever-evolving landscape that is sterile processing, can also result in a lack of knowledge regarding the needs of other positions, and a lack of communication across roles and departments.
Problem number one: effective collaboration. Specialization, while critical for the ever-evolving landscape that is sterile processing, can also result in a lack of knowledge regarding the needs of other positions, and a lack of communication across roles and departments.
It’s Castillo-Gutierrez’ job to identify and solve problems such as these. She frequently audits the sterile processing department at Texas Children’s Hospital for key gaps in education or communication. After identifying important gaps, she partners with all departments to problem-solve and mitigate risk for every silo involved.
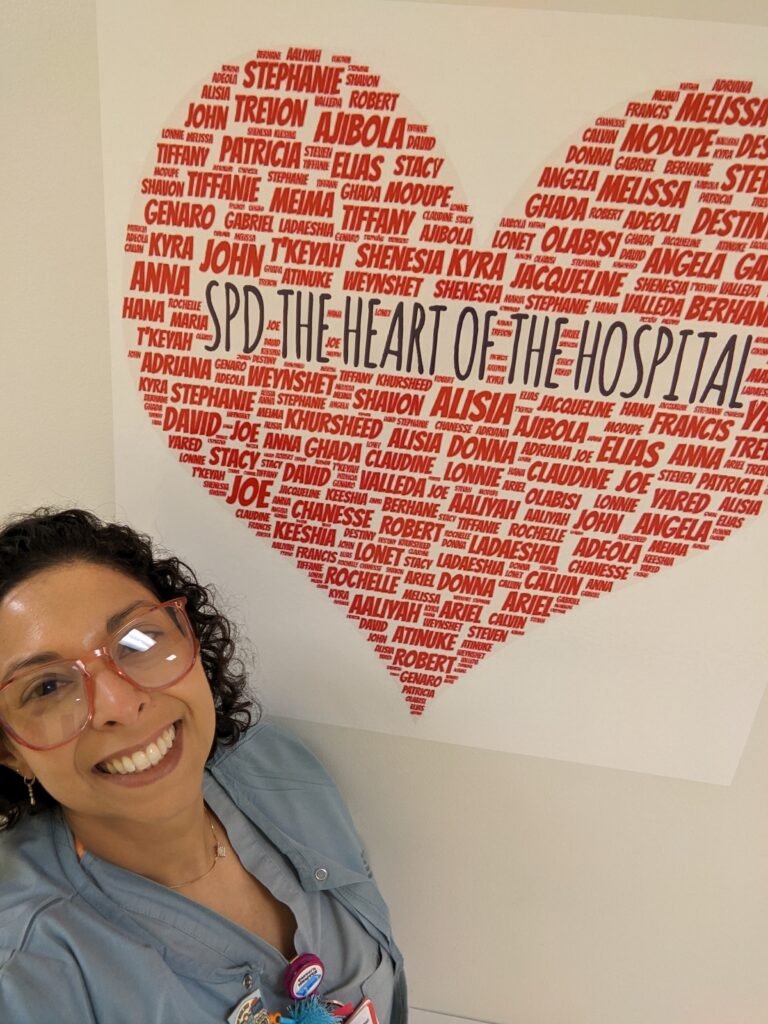
Many solutions, she’s found, are cultural. Castillo-Gutierrez advocates strongly for the importance of fostering a culture based on collaboration.
“One of the most important things that we need to promote is having a culture of safety and teamwork,” said Castillo-Gutierrez. “That’s one of the major gaps that I try to bridge – making sure that the end user of the instrument knows what our processes are in SPD so that realistic expectations are set on both sides of the equation. Partnering with the other departments is key to minimizing a lot of the concerns and the risks that exist in sterile processing.”
Where Individuals Come In: How to Build Processes That Just Make Sense
This kind of education has been a theme in Castillo-Gutierrez’ career. In fact, she began her career as an elementary school educator. “When I started work as a sterile processing technician, I was naturally inclined towards the education part of the job,” said Castillo-Gutierrez. Now, she is a sterile processing educator at one of the largest pediatric hospitals in the United States. She previously held educator and director positions at college institutions such as Fortis College, along with other health systems.
In addition to bridging gaps between departments and specializations, many of the gaps that Castillo-Gutierrez catches and addresses happen on an individual, human-error level.
 “One of the things that I often see are user error mistakes that occur during simple tasks because technicians are overwhelmed or moving too fast,” said Castillo-Gutierrez. “For example, someone labeled an instrument set wrong because they were working on two sets at once, or someone peel-packaged something so quickly that the seal wasn’t correctly sealed. Those small issues are the ones that we tend to identify the most.”
“One of the things that I often see are user error mistakes that occur during simple tasks because technicians are overwhelmed or moving too fast,” said Castillo-Gutierrez. “For example, someone labeled an instrument set wrong because they were working on two sets at once, or someone peel-packaged something so quickly that the seal wasn’t correctly sealed. Those small issues are the ones that we tend to identify the most.”
These “human error” gaps are sometimes the most difficult to correct. Simply reprimanding technicians and nurses for the mistake is not a realistic or effective solution. So, how does one mitigate errors such as these?
“Whenever I identify a gap,” said Castillo-Gutierrez, “I don’t just throw a new process together to fit the agenda of our auditors. I get to the root of the problem, starting by going into the department and trying it out myself. I focus on ensuring that whatever process we are asking our technicians to undergo is user-friendly and makes sense.”
Once she identifies the problem and the solution, that’s where education comes in. As any educator knows, not all pedagogical methods are created equal, and there’s little guarantee that what one is teaching will stick in the brains of one’s students. But a green flag that Castillo-Gutierrez has done her job right, is if she starts to see her students become advocates for the solution she taught.
“I try to deliver education in a way that is so easy that people pick it up almost immediately,” said Castillo-Gutierrez. “The goal is that the solution and the delivery of the solution are good enough that students begin teaching others and advocating for the solution across the department. Once I get someone to the point where they begin helping others and teaching it themselves – that’s how you know a real change has been made.”
Of course, other factors, such as what sterile processing and handling equipment is available, can also make a big difference. A new favorite of Castillo-Gutierrez’ is the robotic arm instrument protector by SterileBits.
The Robotic Arm Instrument Protector has one specific job — to safeguard surgical instruments during sterilization, transport, and delivery to the operative field. Without an instrument protector card, robotic instruments are at risk of damage or compromising the sterile barrier if they pierce the peel pouch at any time during the multiple touchpoints they pass through before reaching the operating room (OR). Not only does this put patient safety at risk, but it’s just another headache for nurses and technicians who must send the instrument for reprocessing.
“I first saw the instrument protector on LinkedIn. I introduced it to my manager, and we’ve been using it ever since,” said Castillo-Gutierrez. “It’s such a lifesaver. I think it’s a great product.”
A New Era of SPD Emerges
All in all, when Castillo-Gutierrez looks to the future of sterile processing, she is thrilled. She sees the energy in the field, an openness to learning, and technological advancements as great signs that the industry is headed to new heights.
“SPD is coming into this neat era where a new generation of young technicians are emerging and elevating the industry,” said Castillo-Gutierrez. “We’re being pretty vocal. My generation of SPD is loud. Technology is evolving so rapidly, and we strive to advocate for our own practices to evolve with it. Practices should be user-friendly and make sense on a fundamental level. That helps push the department forward, not only in our hospitals but in the industry. I’m really optimistic about the industry’s future if we continue to work hard together to find the best – and the easiest – solutions to our problems.”
SterileBits: Filling the Gaps
To read more stories similar to this one, visit the SterileBits blog or follow SterileBits on LinkedIn.

